COVID-19 victims now mostly older or unvaccinated
With COVID-19 cases falling since the Delta variant summer surge, I recently found this information about who is still getting sick. I expected the majority were the unvaccinated, and that's mostly right. Several surveys collected during the August surge point that out -- the risk of dying from Covid-19 was 11 times higher for unvaccinated adults than for fully vaccinated adults and the risk of being hospitalized was nearly 19 times higher. A Kaiser Family Foundation analysis estimates more than 90,000 preventable Covid-19 deaths among unvaccinated adults over the three month Delta surge, with more than half of them occurring in September alone. Several unvaccinated patients told me they feel safe because the had already survived infection with COVID-19. Unfortunately, this proves to be a false hope; plenty of people previously infected were again made ill by the Delta variant. The solution yet again, is getting the vaccine. Consider this study of COVID-19 infections in Kentucky among people who were previously infected with SAR-CoV-2. Unvaccinated individuals are more than twice as likely to be reinfected with COVID-19 than those who were fully vaccinated after previous infection with the virus. COVID-19 vaccines offer better protection than natural immunity alone -- vaccines, even after prior infection, help prevent reinfections.
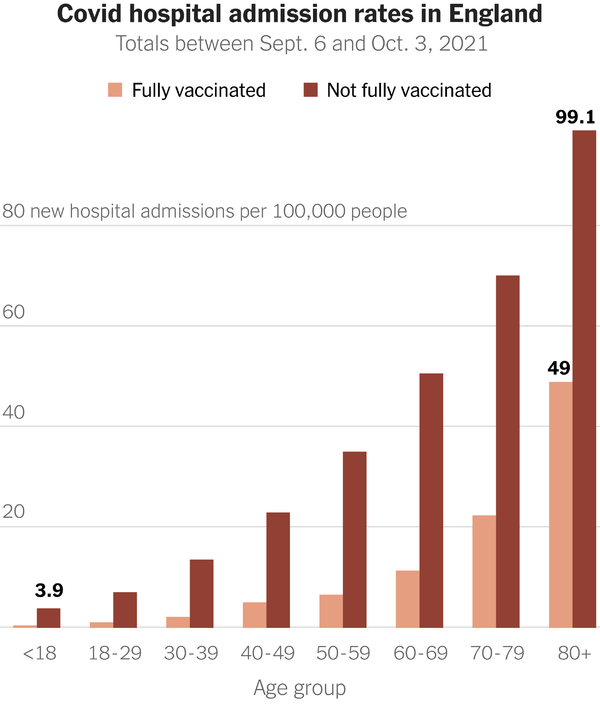
Unfortunately, the virus is not finished with vaccinated seniors either (like me). The graph to the right shows hospital admissions in England, which has a higher vaccination rate among the elderly than the US. As you can see, the risk of COVID-19 infection requiring hospitalization increases substantially with age, even among the vaccinated. Still, getting vaccinated is the best way for seniors to reduce their risk of serious illness or death if they become infected. And it's why I'm telling my older patients to get the booster, and have done it myself. We older Americans should also be prudent -- wear a mask and practice social distancing around other people when inside. Outside is still less risky (but you won't find me at a football game this fall with 90,000 other fans).
Doctors are alert now for acute COVID-19 symptoms: fever, dry cough, malaise, aching, loss of smell or taste, severe weakness and difficulty breathing. But my own experience evaluating some older patients, and a recent study in the Journal of Gerontology, show that some older patients may not have these easily recognizable complaints when infected with the virus. In the study, about one-quarter of older patients showed functional decline: falls, fatigue, weakness, difficulty walking or getting out of bed. Some only had poor appetite, confusion, agitation, forgetfulness or lethargy. Only half had a typical COVID-19 symptom like cough. The importance of being alert to these nonspecific symptoms is that one-third of these seniors who needed hospitalization died. Presumably early recognition and giving monoclonal antibody would have lessened complications.
Hospital admissions, vaccinated and unvaccinated persons by age
The pandemic is not gone, maybe not even weaning. We need to use what we know (i.e.: vaccination and safety measures), & be alert about what we do not know. Stay safe