Electronic Medical Records and Patients
We all have been told for years that conversion of medical records from paper to digital data would improve medical communications, reduce errors, help patient care become more uniform and comprehensive, increase efficiency and save billions of dollars. So why has none of this come to pass? More than a decade since President Bush announced his initiative to introduce technology into medical care, and after spending 30 billion dollars on President Obama's 2009 HITECH (Health Information Technology for Economic and Clinical Health) Act, these goals have not been met.
First, some definitions. An electronic medical record (EMR) is a digital version of a paper chart that contains all of a patient’s medical history from one practice. The information stored in EMRs is not easily shared with providers outside of a single practice. Over 700 different software products are in use, most do not share data with other EMR software. Absurd as this may sound, most medical information is still transmitted between offices by fax, which has been in use since the 1880's. A patient’s record might even have to be printed out and delivered by mail to other doctors.
Electronic health records (EHRs) go beyond the data collected in a single practice and include a more comprehensive patient history. EHRs are designed to contain and share information from all providers involved in a patient’s care. EHR data can be created, managed, and consulted by multiple doctors and healthcare workers from across more than one health care organization. Many large healthcare entities such as hospitals use EHRs to document & manage patient care within the institution, but most still cannot share data with unaffiliated doctors or healthcare organizations.
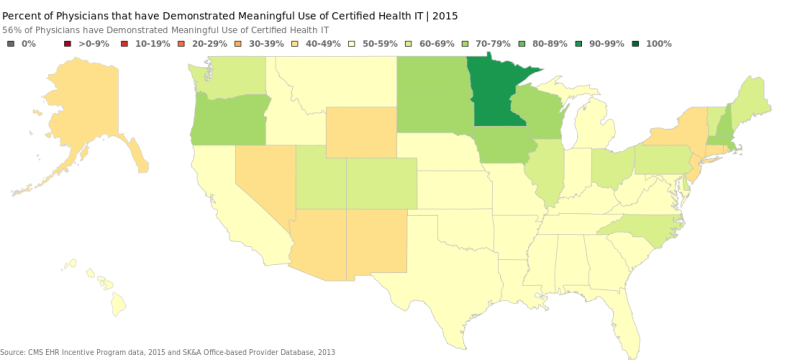
Since 2011, a federal program known as Meaningful Use has offered doctors and hospitals financial payments to adopt electronic records. In it's present form, physicians are now beginning to face penalties for not using digital records. As a result, over 50% of practices are using electronic records.
Health Information Exchange. Despite the increased use of EMRs, exchange of medical data electronically remains abysmally low. Advantages of improved care and avoiding errors and unnecessary duplication of testing will only occur only after the individual EMRs in each physician’s office are interoperable with other physicians offices, hospitals, laboratories or other testing & treatment facilities. Patient electronic access to their doctor and records is also rare. Only 0.2% of patients viewed or downloaded their health information electronically in 2014.
Interconnectivity has proven the most difficult aspect of successful use of electronic records. There are technological hurdles in having systems engineered by different companies interconnect because of variations in operating systems & database structures. For business reasons, vendors consider their software proprietary, and are unwilling to interface with other companies’ products.
Health Information Exchanges (HIE) were proposed to form an interface between incompatible EMRs. Although HIEs exist in every state, most are poorly funded and infrequently used, and have not been self sustaining once federal start-up grants are expended. Numerous hurdles of costs, technologic challenges, economic competition have not been addressed.
Data privacy. The transition from paper to digital records has made often spectacular thefts of protected health information (PHI) commonplace. Forbes Magazine quotesthe IDC’s Health Insights group prediction that 1 in 3 health care recipients will be the victim of a health care data breach in 2016.
Financial and Interactional Costs of Implementing EHRs. HealthIT.gov quotes several studies of the cost of purchasing and installing an electronic health record (EHR) ranging from $15,000 to $70,000 per doctor. In addition, using EMRs reduces efficiency. Research by Michael Howley examining thirty ambulatory practices for two years after EMR implementation found that, on average, productivity declined by an average of 15 patients per physician per quarter. EMRs require doctors (not great typists), not transcriptionists (paid much less), to enter data from patient encounters. Patients lose interaction time with doctors; according to a Northwestern university study, physicians with EHRs in their exam rooms spend one-third of their time looking at computer screens, compared with about 9% using paper charts.
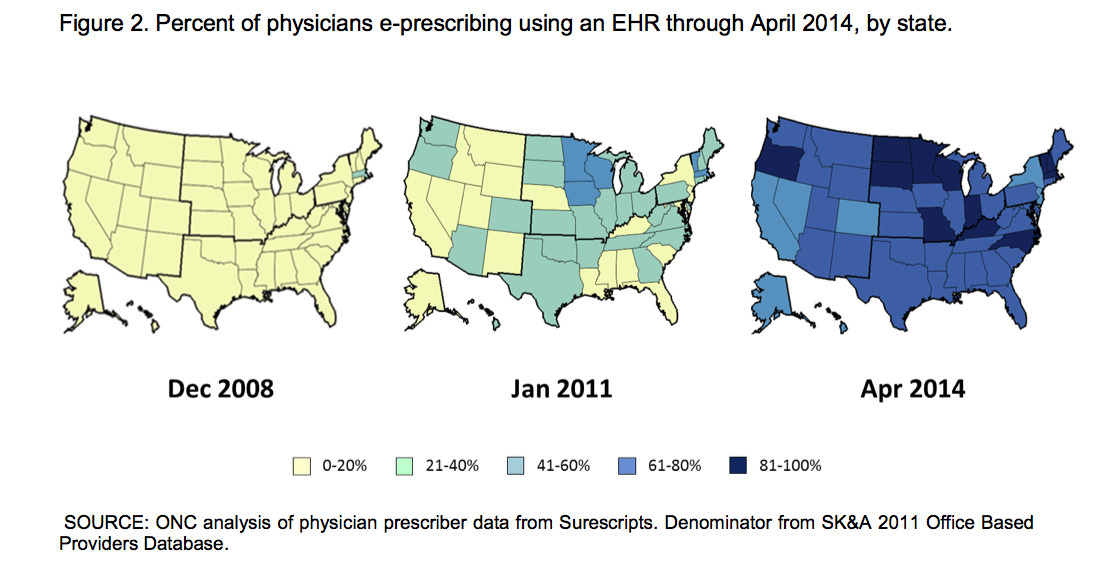
The EMR future. Where do patients and doctors go from here? Certainly there are some bright spots. Electronic prescribing has improved convenience and efficiency for patients & medical staff, and successfully overcome doctors' legendary poor handwriting to reduce prescribing errors.
There is likely to be an increasingly prominent role for patient electronic access to physicians & records. While this may be welcomed by some, many patients will struggle with non-traditional means of making appointments, refilling prescriptions, contacting their doctors, getting approval for tests & treatments and retrieving results. I have already had many comments from my patients about these issues. New payment models for Medicare (such as MIPS, which I have written about in a previous blog post) suggests the federal government’s commitment to addressing the country’s health care cost challenges are experimental models, on a sweeping scale, without patient & physician input. Doctors are required involve patients electronically, willingly or not, to meet mandates. Certainly there is little value for patients, since true interoperable EMRs do not exist. But recent comments by Andy Slavitt, head of the Center for Medicare & Medicare (CMS) indicates more of the same tech burdens in store for doctors & patients.
Due to the controversy of these new proposals, CMS has extended the public comment period on proposed requirements for additional technology use until November 17, 2016. If you don't want to be a test subject in your own healthcare experiment, I suggest making a comment now.