Reduced Medicare Payments to Doctors: How Will It Affect Patients?
Effective January 2017, physicians accepting Medicare assignment (96% of doctors nationwide) will be required to participate in the Merit-Based Incentive Payment System (MIPS). Physicians are scored on quality, "advancing care information" (using health technology), clinical practice improvement activities and (surprise!) saving Medicare money. Doctors with high scores have lowered Medicare payments 4% beginning 2019, and as much as 9% by 2022.
Objections from primary care doctors have been numerous & vocal. Scoring focuses on preventive screenings, cost savings and use of testing, but important aspects of primary care such as physician-patient communication and making timely and accurate diagnoses are not counted.
Patients should expect the following consequences of yet another government attempt to "reform" the healthcare system:
Vanishing Private Practice Doctors: As a result of the new payment structure, the government office for Medicare, the Center for Medicare services (CMS) itself estimates that over 80% of small private doctors offices will face reduced payments in 2019.
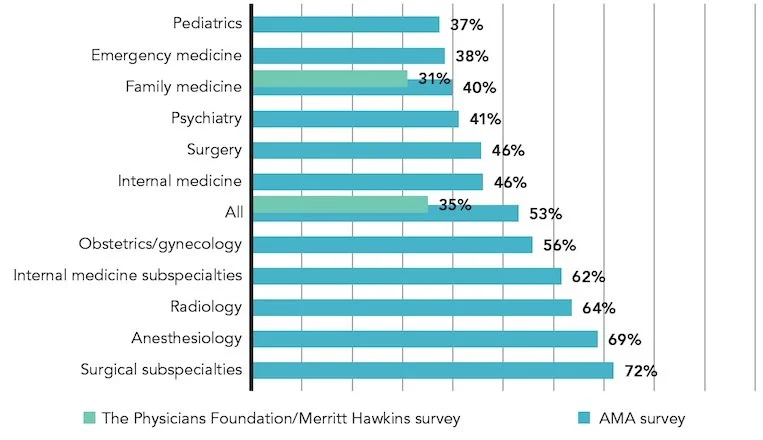
This is likely to accelerate the trend of doctors abandoning private practice to work for hospitals or large groups. The percentage of self employed physicians has already dropped from 62% down to 35% since 2008.
For Medicare and patients with Medicare, losing your independent physician is bad news. According to Atlantic Magazine:
By buying a physician practice, a hospital can charge more for the same test or procedure, even though it is performed in the same place by the same physician. In some cases, such "facility fees" can raise prices to Medicare by as much as 70 percent compared to what would be paid to an independent physician.
Higher Costs for Medicare Patients: Small practices are also likely to try to recover lost income by changing from accepting assignment (i.e.: full payment from Medicare) to non-participation. "Non-par" doctors may charge the patient 15% over Medicare fee schedule and, although they file Medicare charges, the patient will have to wait for Medicare to repay them and be responsible for the balance:
Growth of Concierge Medicine: A recent survey found other practice trends, with 7% of doctors now requiring patient retainers (concierge or direct pay model) of up to $1,500 per year, and additional 13% planning to transition to direct patient payments, including 17% of younger physicians.
Non-Physicians Providing Care: As independent physician practice is succumbing to the dual pressures of reduced fees and burdensome payment systems, it is likely that health care of America's aging population will be increasingly by a non-physicians, either a Physicians Assistant (PA) or Nurse Practitioner (NP).
Gaming the Scoring System: Using the measures proposed by CMS, sicker patients will have to be avoided, since they will drag down quality measures and have increased costs of care, both of which will subtract from a doctors MIPS score. David Hogberg, a senior fellow at the conservative National Center for Public Policy Research writes:
It can be expected that MIPS scoring will encourage physicians to “game the system” by eschewing sicker patients. They will avoid ... patients who need much more encouragement and monitoring, since taking on too many of those patients could result in a below average score ... and, hence, a penalty. MIPS will also incentivize the most talented physicians to pursue the least challenging avenues of medicine. The least challenging areas of health care will be the ones where it will be easiest to achieve high scores on quality measures and thus receive bonuses.
Ultimately, the sickest patients will suffer as MIPS incentivizes the best physicians to avoid them.
Concerned? Then Act! Although these trends are already established, previous decisions by CMS have gone awry and have been reversed. Patient input is important, Medicare and also state and national elected officials listen to grievances and can effect change.