Should men get a Prostate Specific Antigen (PSA) test?
It's undeniable that detection of prostate cancer can save more lives, but the best process for screening may be less clear. For example, testing using Prostate Specific Antigen (PSA) tests could help detect cancer early, but others note serious doubts.
PSA is a protein enzyme present in low levels in the blood of men with healthy prostates, but it is elevated in the presence of prostate cancer and other benign prostate disorders. In 2012, the U.S. Preventive Services Task Force (USPSTF) recommended against using PSA to screen for prostate cancer. Screening is defined as testing a man who has no symptoms of prostate cancer. This recommendation was based on combining data from several medical studies showing PSA screening resulted in no significant reduction in death from prostate cancer. Aggressive treatment of asymptomatic prostate cancer has not been shown to benefit patients, and may cause harm. The USPSTF has published a FAQ for patients about the recommendation.
African-American men and men with a family history of prostate cancer have an increased risk of prostate cancer. Prostate cancer is not only more common but also more aggressive in African-American men. Studies are not definitive, but it has been suggested that the recommendation against PSA screening should not apply to these higher risk men, since early diagnosis may be beneficial.
How has this recommendation affected the detection of prostate cancer?
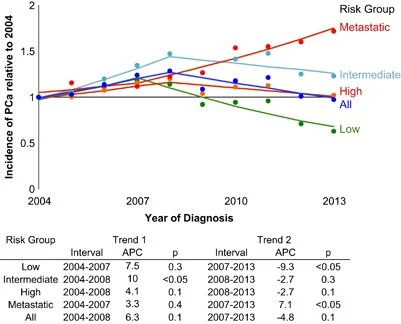
Since 2012 fewer patients have had PSA screening. During this same period, there has been an increase in metastatic prostate cancer, that is, cancer spread outside the prostate gland at the time of diagnosis. This increase in metastasis is highest in men age 55-69, in whom active surveillance or treatment of prostate cancer has the most benefit.
The USPSTF is presently studying whether the recommendation against PSA testing of asymptomatic men needs revision, based on this increased rate of advanced prostate cancers.
Image above is from Prostate Cancer and Prostatic Disease (2016) 19, 395–397; doi:10.1038/pcan.2016.30; published online 19 July 2016.
Tragically, in 2025 ex-president Joseph Biden was diagnosed with aggressive prostate cancer, already spread to bones. The prognosis is poor for cure because of the advanced state at which the cancer was detected. Noteworthy in the news reports, was that the ex-president, despite what one would assume would be the highest level of medical care available, had not had a PSA test done for over 10 years. This is of course consistent with FDA recommendations, but in my opinion Mr. Biden's cancer would have been detected before it had spread to his bones if annual PSAs had been continued.
My Recommendation for Detecting Prostate Cancer
Because I am concerned about this trend, I recommend that a man between age 50-75, who has at least a 10 year life expectancy, obtain a PSA for screening. A PSA is also needed if he is having a symptom related to urination, or is in an elevated risk group. Obtaining the PSA test is not to make a diagnosis, it is to open a discussion about the meaning of the result, and whether further testing is needed.
I am not convinced that PSA tests are the best way to detect prostate cancer, but as the USPSTF reviews this recommendation, the medical community continues to seek better screening tests. There are promising new developments in prostate cancer screening. Researchers in London from the Prostate MRI Imaging Study (Promis) have developed multi-parametric MRI (mpMRI). This scan detects twice as many aggressive prostate cancers as prostate biopsy with none of the risks associated with biopsy.
Image above is from Prostate Cancer and Prostatic Disease (2016) 19, 395–397; doi:10.1038/pcan.2016.30; published online 19 July 2016.